Blood vessels connecting to whole-brain organoids can further develop study of brain, vessel diseases
Researchers at the Institute for Regenerative Cures at UC Davis may have solved one problem facing the future of stem cell brain models. A recent paper proved it was possible to introduce blood vessels into whole-brain organoids using endothelial stem cells, potentially unlocking new ways to study diseases the brain and its blood vessels.
Whole-brain organoids are models of brain and neural tissue created by scientists using induced pluripotent stem cells. The stem cells are given chemical signals, which coax them into developing as neural cells for scientists to study brain functions in an easily controlled environment.
One problem with the neural organoid process is that the tissue originally has no blood vessels within it. Since oxygen and nutrients cannot reach the organoid core through diffusion, the center of the cellular mass tends to die after reaching a certain size and being unable to meet its energy needs. But with blood vessels, made from endothelial stem cells, bringing nutrients into the cells and removing waste, a way of keeping organoids alive longer may be within reach. A UC Davis patient volunteered some of their cells for this project.
“The original cell type was a dura fibroblast that was isolated during shunt surgery from a UCD patient,” said Whitney Cary, the director of the UC Davis Stem Cell Core, in an email interview. “The patient had agreed to donate this tissue to our work as it would have been discarded normally during the surgery.”
The fibroblasts from the UCD patient’s brain lining were split into two groups. One group of stem cells were selected to form the whole-brain organoid, while the other group grew into endothelial cells. Even though both group of cells came from the same patient and the same fibroblast cell type, researchers were able to grow them into entirely different types of cells based on the cell culture media, protocols and environments involved.
“There are different medias out there, and finding the best one for your particular cell type takes some experimenting,” said Missy Pham, the first author of the study, in an email interview. “For the most part, companies have already figured this out for us, but even then, each company has their own unique formulation. For our iPSC culture, we are still testing new medias all the time and switching based on what our cells grow best in.”
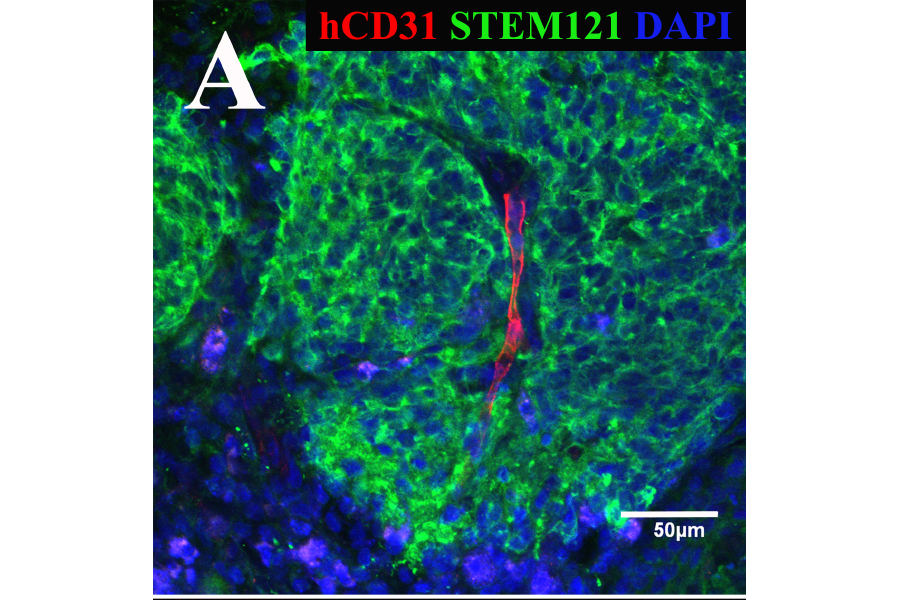
After coating the organoid with the endothelial cells, the endothelial cells immediately began to coalesce to form tubular structures and then capillaries. The cells grew separately for 34 days, 20 days with endothelial cells coating the whole-brain organoid, and finally two weeks surgically implanted in a mouse brain. The organoids were extracted on day 68 of the experiment and were shown, through fluorescent staining, to contain a protein known as CD31, which is only found in human blood vessels. Together, a vascularized whole-brain organoid was proved possible, created completely through the stem cells of one patient.
“But we haven’t shown these blood vessels are actually functional,” said Dr. Ben Waldau, an associate professor of clinical neurosurgery at UC Davis Medical Center and the project leader. “We haven’t shown that they have a functional blood brain barrier. We haven’t shown they are actually perfused with blood.”
Enabling blood to flow through a whole-brain organoid is the first of many steps needed to improve the model. With a steady blood supply, larger and more sophisticated organoids could possible be developed, allowing more complicated research and medical diagnostics to be practiced on brains in cell culture formats instead of live human patients.
“We are one of the first groups to show organoids can be vascularized with blood vessels,” Waldau said. “It looks like they are still healthy and their structural organization does not seem to be disturbed. The most exciting thing about the paper is this may open an avenue in the future to study the blood brain barrier in an organoid, which is huge. There are so many diseases where the blood brain barrier is disturbed and pharmacological testing would be important.”
Written by: George Ugartemendia — science@theaggie.org