Researchers have got a first look at phase III clinical trial data for a much lauded experimental Alzheimer’s drug—and although the data support it having a moderate cognitive benefit for people, scientists worry about its safety.
The results, presented on 29 November at the Clinical Trials on Alzheimer’s Disease conference in San Francisco and simultaneously published in the New England Journal of Medicine, confirmed that the treatment, a monoclonal antibody called lecanemab, slowed cognitive decline by 27% relative to placebo in an 18-month study of nearly 1,800 participants. The antibody’s developers—pharmaceutical firm Eisai, based in Tokyo, and biotechnology firm Biogen, based in Cambridge, Massachusetts—announced these topline findings in September in a press release.
But the disclosure comes amid media reports that lecanemab might have contributed to the deaths of two people who had participated in the trial—adding to an ongoing debate over whether the experimental drug’s modest benefit is worth its accompanying safety risks. Eisai has denied lecanemab played a part in one death, and has yet to determine if it had a role in the other.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
“It’s quite a complicated balancing act for risks and benefits,” says Rob Howard, a psychiatrist at University College London who specializes in dementia. And he worries about how patients and families who are desperate for Alzheimer’s treatments will weigh the two sides, if lecanemab is approved by regulatory agencies.
“All the available safety information indicates that lecanemab therapy is not associated with an increased risk of death overall,” Eisai said in a 29 November statement.
If a connection between lecanemab and the deaths is found, it could pose “a real conundrum” for the US Food and Drug Administration (FDA) as it decides how to rule on lecanemab, says Caleb Alexander, an internal-medicine specialist and epidemiologist at the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland, and an advisory committee member for the FDA. The FDA is slated to decide on whether to give the experimental drug special authorization in early January.
Benefits and risks
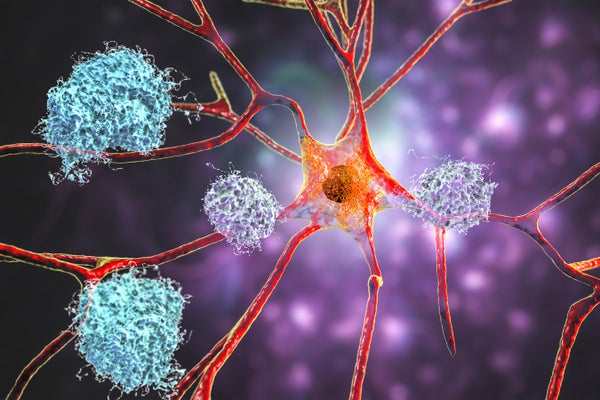
Researchers are glad to see the swift publication of the lecanemab trial data. Some have previously criticized the rollout of another monoclonal antibody treatment for Alzheimer’s: aducanumab. Like lecanemab, aducanumab was designed to sweep clumps of a protein called amyloid-β from the brain; many researchers think this protein is a root cause of Alzheimer’s. The FDA controversially approved aducanumab, which was also developed by Biogen, last year on the basis that it cleared amyloid from people’s brains, but without clear evidence of cognitive benefit.
By contrast, lecanemab is the first of its kind to slow mental decline in a robust clinical trial. During the trial, called Clarity AD, clinicians administered the treatment to a cadre of people in more than a dozen countries with early-stage Alzheimer’s. Half received biweekly intravenous infusions of lecanemab, while the others received a placebo. Scientists assessed people’s cognition primarily with a metric called the Clinical Dementia Rating–Sum of Boxes (CDR-SB), which evaluates a person’s abilities in six areas, including memory and problem solving, using an 18-point scale.
After 18 months, participants receiving lecanemab scored, on average, 0.45 points better on the CDR-SB than those receiving placebo. Other cognition tests used in the study echoed these results, and the treatment group showed a reduction in amyloid and other disease biomarkers.
But some researchers have questioned whether this shift is big enough to be noticeable in a person. A one-point difference on the CDR-SB is the minimum to be clinically important, Howard says.
“It’s a modest benefit,” says Brent Forester, director of the Geriatric Psychiatry Research Program at McLean Hospital in Belmont, Massachusetts, who helped to run the clinical trial for lecanemab. His concerns lie with safety. About 20% of people receiving lecanemab had brain-scan abnormalities that indicated swelling or bleeding—although less than 3% of those who received the antibody experienced symptoms related to these abnormalities.
This safety profile is better than that of aducanumab. Forty per cent of people receiving that antibody in phase III clinical trials showed brain swelling in scans. But Forester still worries, because if approved, lecanemab would be given to relatively high-functioning people who happen to be in the early stages of Alzheimer’s. Complications might therefore worsen their quality of life.
During Clarity AD, 13 people taking lecanemab developed symptomatic brain bleeds—or strokes—whereas only 2 people in the placebo group did, according to the conference presentation. This represents just 1.4% of the treatment group, Howard says, but “that’s not a trivial risk profile”.
Further exploration needed
Both deaths reported in the media occurred during Clarity AD’s ‘open-label extension’, a period during which a trial has formally ended, but participants who were receiving placebo can opt to receive the experimental treatment. Both involved stroke-related complications.
In one case, reported by STAT News, a participant who used a prescribed anticoagulant, or ‘blood thinner’, for a heart condition, died after a heart attack and four mini-stroke-like events. The other individual, reported by Science, died from a brain bleed after she received an emergency stroke medicine. As reported by both outlets, scientists think it’s plausible that lecanemab could have weakened the brain’s blood vessels by sweeping away amyloid protein lining the vessels in these people’s brains. The medications could have then helped trigger bleeding.
Because of the tie with anticoagulants and other factors, it’s a bit difficult to detangle whether lecanemab played a role in the deaths, said Marwan Sabbagh, a neurologist at the Barrow Neurological Institute in Phoenix, Arizona, while presenting data at the conference. “These things are continuing to be explored,” he said. Although the rate of brain hemorrhage is low with lecanemab, it does rise with anticoagulants, he added.
“I honestly would be in the camp of not prescribing monoclonal antibodies to people on anticoagulation [medicines],” says Liana Apostolova, a neurologist at the Indiana University School of Medicine in Indianapolis who has consulted for Eisai and Biogen.
Whether or not the deaths will affect the FDA’s decision on lecanemab, scheduled for 6 January, is “anybody’s guess”, Alexander says. The agency will consider whether it should grant the drug candidate ‘accelerated approval’ on the basis of phase II clinical trial data showing that lecanemab clears amyloid-β from the brain. The approval would be conditional on Eisai and Biogen conducting follow-up studies to confirm a clinical benefit, which Clarity AD should fulfill.
If lecanemab is approved, Forester says, “I would suspect that there will be recommendations for careful monitoring”.
This article is reproduced with permission and was first published on November 30 2022.